Medical research funding is a critical pillar in the advancement of healthcare, significantly impacting patient safety and the ethical conduct of research. When funding is disrupted, as seen recently with the halt of over $2 billion in federal grants to institutions like Harvard, the integrity and oversight of clinical studies can be severely compromised. This unfortunate scenario not only delays crucial research but also endangers the welfare of patients who participate in these studies, underscoring the symbiotic relationship between research ethics and funding. The role of Institutional Review Boards (IRBs) becomes paramount in safeguarding participant rights and minimizing risks, a process that relies heavily on sound financial backing from entities such as the NIH. Without adequate funding, the ability to monitor, evaluate, and support clinical research diminishes, ultimately affecting public trust in medical innovations and the commitment of researchers to ethical standards.
The financial support for medical inquiries often functions as the bedrock of innovation within healthcare systems, directly tied to ensuring patient safety and ethical adherence. When investments in research initiatives are interrupted, the repercussions are felt across the spectrum of clinical investigations and trials, creating a cascading effect on the oversight provided by crucial entities like Institutional Review Boards. These boards are responsible for protecting the well-being of participants and maintaining standards that govern human subject research, but they depend on resources to function effectively. The cancellation or suspension of NIH grants can halt collaborative efforts, disrupt the integrity of ongoing studies, and raise ethical concerns that can tarnish public perception of medical research. Thus, reliable funding is essential not just for scientific discovery but also for upholding the ethical principles that guard the interests of those involved in research.
The Importance of Medical Research Funding
Medical research funding is vital for the advancement of healthcare and the improvement of patient outcomes. In recent years, federal funding has played a crucial role in supporting innovative studies that can lead to breakthroughs in treatment and prevention. The halt in federal funding, particularly under the Trump administration, has disrupted many projects that were designed to enhance patient safety. Research institutions rely on these funds not only for conducting experiments but also for maintaining IRB oversight, which ensures the ethical treatment of participants in clinical trials.
Without adequate medical research funding, the risks to patient safety increase significantly. Studies require rigorous oversight to ensure that all ethical guidelines are followed, and that’s where funding supports the establishment of necessary protocols and personnel. The scenario where multiple research sites can collaborate effectively under a streamlined oversight system like SMART IRB becomes jeopardized without the necessary financial resources. This can lead to increased delays in critical trials and ultimately, slower progress in finding effective therapies for conditions that severely impact patient lives.
How IRB Oversight Safeguards Patient Safety
Institutional Review Boards (IRBs) are fundamental to ensuring that clinical research studies uphold the highest standards of ethics and participant safety. These boards review research protocols to ascertain that risks are minimized and that participants are clearly informed about the nature of the study, any potential risks, and their rights. By providing informed consent procedures and monitoring the safety of participants throughout the study, IRBs serve as a protective measure against unethical medical experimentation.
Moreover, IRBs play a key role in mitigating risks associated with clinical research. They conduct ongoing assessments of studies, ensuring compliance with applicable regulations, and intervening if adverse events occur. This vigilant oversight fosters trust in research practices, encouraging more patients to participate in clinical trials, ultimately leading to advancements in medical knowledge. The support for IRBs through proper funding is essential, as it allows them to maintain their integrity and functionality in the face of evolving research demands.
Impact of Funding Cuts on Research and Ethics
Funding cuts have a direct and detrimental impact on research ethics and patient safety in clinical trials. With the reduction of financial resources, institutions may struggle to maintain necessary IRB oversight and compliance with ethical research standards. This not only hampers ongoing studies but can also result in potential harms to participants if studies are conducted without thorough ethical scrutiny. The credibility of the research community is put at risk, leading to increased skepticism among patients and the public towards participating in clinical trials.
Furthermore, historical examples of unethical research underscore the need for stringent oversight systems that are fully supported by adequate funding. Events such as the Tuskegee syphilis study reveal the consequences of insufficient oversight, showcasing the critical nature of ethics in research. As funding for IRBs and ethical review processes diminishes, the specter of past abuses looms larger, potentially reversing the progress made in enhancing patient protection through comprehensive regulation and oversight.
The Role of NIH Funding in Research Advancement
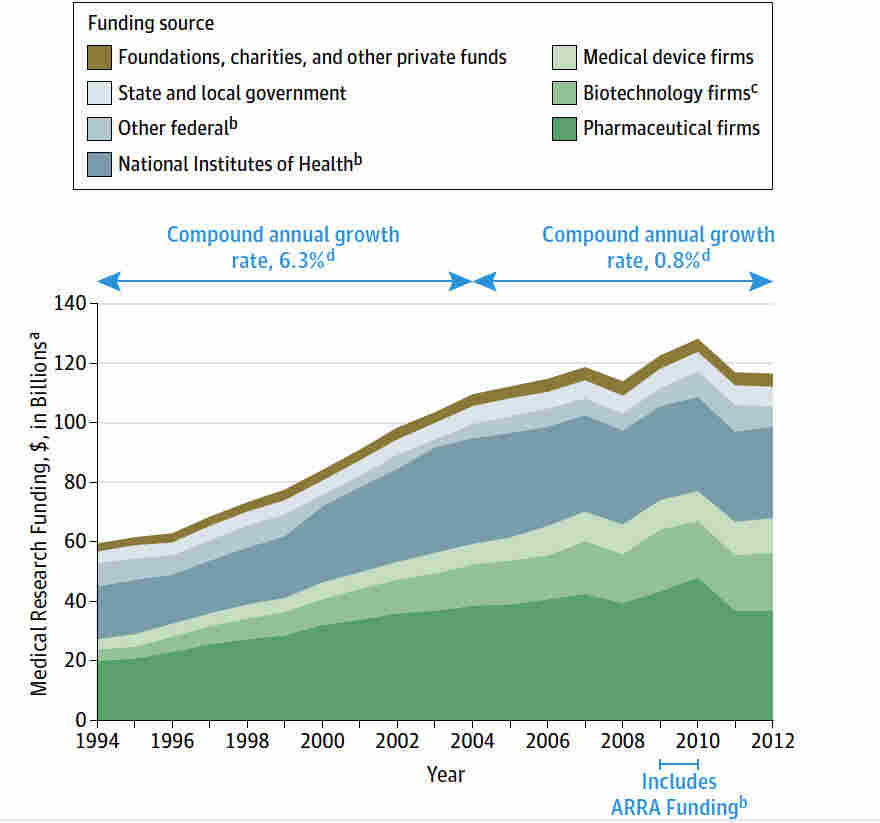
NIH funding is a cornerstone for many high-impact medical research studies. This federal support not only helps cover the costs of conducting research but also provides necessary funds for IRB oversight, ensuring that all studies are ethically sound. NIH grants facilitate a better understanding of human diseases and treatments, enabling researchers to conduct vital work that could lead to significant healthcare advancements. With cuts in NIH funding, innovative projects may be stalled or entirely canceled, hindering progress in areas crucial to patient care.
In addition, the collaborative nature of modern clinical research relies heavily on NIH support to unite various institutions and coordinate multi-site studies efficiently. Without this funding, researchers face barriers to collaboration, creating a fragmented research landscape that limits the potential for groundbreaking discoveries. The reliance on a single IRB for multi-center studies, as required by NIH policies, is compromised when funding is cut, reinforcing the critical need for sustained investment in research initiatives that prioritize patient safety and ethical standards.
The Historical Context of Research Ethics
Understanding the historical failures in research ethics provides a framework for appreciating the importance of institutional oversight in clinical studies. Historical events, like the Tuskegee study and the breaches of informed consent, have significantly shaped the ethical landscape of medical research. They are reminders of the potential risks and harms that can occur when patient welfare is not prioritized, leading to the establishment of stringent guidelines and regulations overseen by IRBs. These safeguards are designed to prevent any recurrence of such unethical practices and ensure patient safety.
In response to such dark chapters, the field of bioethics has evolved with a mission to uphold human dignity in research. Modern IRB systems emerged as a protective measure to instill public confidence in clinical research. Historical lessons underscore the significance of sustained funding in bolstering these review boards and ensuring that ethical standards are maintained. As medical research progresses, the lessons of history must guide funding decisions to avoid repeating mistakes of the past and to ensure robust protections for research participants.
Community Engagement in Clinical Research
Community engagement is increasingly recognized as a vital component of clinical research, fostering trust and collaboration between researchers and study participants. Engaging communities in the research process ensures that studies address relevant health issues and that participants feel valued and respected. This helps dismantle barriers that may prevent individuals from participating in clinical trials, ultimately leading to a more diverse and representative sample of research subjects. However, without adequate funding for community outreach initiatives, these efforts may dwindle, impeding progress in clinical studies.
Additionally, community involvement allows for deeper insights into the concerns and needs of potential participants, thus enhancing informed consent processes. When participants understand how research directly relates to their health and well-being, it cultivates a sense of partnership in the research, ultimately leading to better patient safety outcomes. Continued investment in community engagement strategies is essential for ethical research conduct, ensuring that studies reflect the communities they aim to serve, thereby boosting patient safety and trust.
The Future of Clinical Research Amid Funding Cuts
The landscape of clinical research is experiencing profound changes due to funding cuts that threaten to stifle innovation and jeopardize patient safety. With many studies placed on hold or entirely canceled, researchers face mounting challenges in making progress toward public health goals. The commitment to ethical research and the safety of participants is increasingly strained, as IRBs struggle to maintain oversight without proper financial support. This situation demands urgent attention from policymakers to prioritize investment in medical research funding.
As the future of clinical research hangs in the balance, it is imperative to advocate for sustained funding initiatives that not only support innovative therapies but also fortify the ethical foundations of research. The collaboration among funding agencies, research institutions, and regulatory bodies is crucial for advancing patient safety standards while ensuring continuous growth and integrity in the research community. By reinforcing these pillars, we can ensure that clinical research remains a trusted endeavor that prioritizes the health and well-being of all participants.
The Ethical Imperatives of Medical Research
Ethics in medical research are paramount to ensuring the safety and rights of participants. Researchers have a moral obligation to conduct studies responsibly, returning benefits to the communities that contribute to research findings. This principle requires an adherence to rigorous ethical guidelines and comprehensive oversight from IRBs, which serve as guardians of participant welfare. Enhancements to research ethics derive from historical failures, reminding us that vigilant oversight is necessary to protect the rights of individuals involved in studies.
Furthermore, ethical medical research fosters public trust, encouraging participation in clinical trials necessary for advancing health care. When funding remains stable, institutions can maintain the ethical frameworks and IRB oversight that solidify this trust, ensuring patients feel secure in the research process. This trust is vital for the recruitment and retention of participants, thereby enhancing the overall quality of clinical research and its societal impact.
Ensuring Patient Rights and Welfare in Research
Central to the discussion about medical research is the need to ensure the rights and welfare of patients involved in studies. Clear articulation of patient rights is essential for informed consent processes, empowering individuals to make educated decisions about their participation in research. Conversely, institutions must establish comprehensive measures to safeguard these rights, and that requires adequate funding to implement necessary oversight and ethical practices. Strong, well-financed IRB systems serve to uphold these standards, demonstrating the necessity of stable funding for medical research.
The protection of patient welfare isn’t solely a regulatory issue but also an ethical commitment intrinsic to the research community. Researchers must constantly reassess their methods to ensure they align with best practices that prioritize patient safety. This ongoing commitment can only be fulfilled with sustained financial support for research ethics training, oversight resources, and participant engagement initiatives. As we navigate future research landscapes, these efforts will be crucial in safeguarding the interests of patients and preserving the legitimacy of the research enterprise.
Frequently Asked Questions
How does medical research funding ensure patient safety during clinical trials?
Medical research funding plays a critical role in ensuring patient safety during clinical trials by supporting the operations of Institutional Review Boards (IRBs). These IRBs are responsible for reviewing research proposals to protect the rights and welfare of research participants. By providing necessary funding, agencies like the NIH enable comprehensive oversight and monitoring, which are essential to maintaining high standards of safety and ethics in clinical research.
What are the implications of NIH funding cuts on clinical research ethics?
NIH funding cuts can severely affect clinical research ethics by limiting the resources available for IRB oversight and the ethical management of studies. Reduced funding may lead to less comprehensive review processes, putting research participants at risk and undermining the integrity of research ethics. Such setbacks in funding could diminish public trust in medical research and compromise patient safety across various studies.
In what ways do IRBs facilitate safe practices in medical research?
Institutional Review Boards (IRBs) facilitate safe practices in medical research by rigorously evaluating research designs, ensuring informed consent processes are followed, and monitoring for adverse events. Their oversight is funded through medical research grants, which highlight their vital role in protecting patient safety by adhering to ethical standards throughout the research process.
How can a halt in medical research funding disrupt studies focused on patient safety?
A halt in medical research funding can disrupt studies focused on patient safety by preventing research institutions from maintaining oversight and compliance with ethical standards enforced by IRBs. When funding is cut, projects may face delays, new sites cannot join ongoing trials, and the ability to monitor participant safety and rights diminishes, thereby risking harm to those involved in clinical research.
What historical events highlight the importance of research ethics in medical funding?
Historical events, such as the Tuskegee syphilis study and unethical medical experimentation during World War II, underscore the importance of robust research ethics in medical funding. These incidents led to heightened awareness and the establishment of IRBs, ensuring that patient safety is prioritized in clinical research. Funding for research ethics initiatives is essential to prevent past mistakes from reoccurring and to maintain the public’s trust in medical research.
What is the SMART IRB and how does it relate to NIH funding?
The SMART IRB is a national system designed to streamline the review and oversight of multisite research studies. It receives funding from NIH grants, which supports its operations and allows for collaborative research across multiple institutions. By facilitating IRB processes, SMART IRB helps ensure that patient safety and ethical standards are upheld in clinical trials, demonstrating the critical link between NIH funding and effective oversight in medical research.
| Key Point | Details |
|---|---|
| Funding Freeze | Trump administration’s halt of $2 billion in federal grants disrupts patient safety efforts. |
| Impact on Oversight | Stop-work order prevents addition of new clinical sites, affecting ongoing medical studies. |
| Role of IRBs | IRBs ensure participant protection by reviewing study designs and managing risks of harm. |
| Historical Significance | Events like the Tuskegee study led to the establishment of oversight systems for medical research. |
| Future of Research | Funding cuts risk public trust and can halt advancements in scientific research. |
Summary
Medical research funding is critical for protecting patient safety and ensuring ethical oversight of clinical studies. The recent halt in funding has significant implications for ongoing research and participant welfare. Without adequate financial support, essential safety measures governed by Institutional Review Boards (IRBs) are at risk, which could lead to harmful outcomes in medical research. It is vital to address these funding issues to uphold the integrity of medical research and safeguard participants.