Predicting brain cancer recurrence, especially in pediatric patients, is a critical area of research that aims to enhance treatment outcomes and reduce the burden of ongoing monitoring. A groundbreaking study from Harvard highlights the power of AI in cancer prediction, demonstrating a notable improvement in relapse risk assessments over traditional methods. By analyzing multiple brain scans through a novel approach known as temporal learning, researchers have significantly boosted the accuracy of predicting the recurrence of pediatric gliomas, a type of brain tumor. This advancement in brain cancer imaging not only provides hope for timely interventions but also aims to mitigate the stress associated with frequent imaging for young patients. As the medical field embraces AI in cancer prediction, the potential for personalized treatment plans becomes ever more attainable, paving the way for a brighter future in pediatric oncology.
The challenge of assessing the likelihood of brain tumors returning, particularly in children, calls for innovative strategies in cancer monitoring. Alternative terms such as tumor recurrence evaluation and pediatric brain tumor monitoring emphasize the importance of effective assessment mechanisms. Recent advances in artificial intelligence have introduced promising methodologies in predicting the probability of reemergence using longitudinal imaging data. These enhancements in risk analysis for pediatric gliomas offer new pathways for tailoring care and improving patient experiences. As we continue to explore these cutting-edge approaches, the landscape of pediatric cancer care stands poised for transformation, with an emphasis on precision and patient-centric solutions.
Understanding Pediatric Gliomas and Their Treatment
Pediatric gliomas represent a diverse group of brain tumors that primarily affect children. These tumors arise from glial cells in the brain and spinal cord and can range from benign to aggressive types. Treatment options for pediatric gliomas often involve surgery, which can effectively remove the tumor, especially in cases where it is detected early. However, one of the critical challenges in managing pediatric gliomas is the risk of recurrence. Even when children achieve remission, the possibility of relapse can loom over families, making ongoing monitoring essential.
The prognosis for pediatric glioma patients varies significantly based on tumor grade and location. While many low-grade tumors can be cured with surgery alone, high-grade gliomas pose a greater challenge, often requiring additional treatments such as chemotherapy and radiation. The psychological impact on children and their families during this tumultuous journey toward recovery is substantial. Hence, advancements in predictive tools that can assess recurrence risk effectively are crucial. Research efforts focused on enhancing brain cancer imaging technologies are vital in improving clinical outcomes for these young patients.
The Role of AI in Cancer Prediction
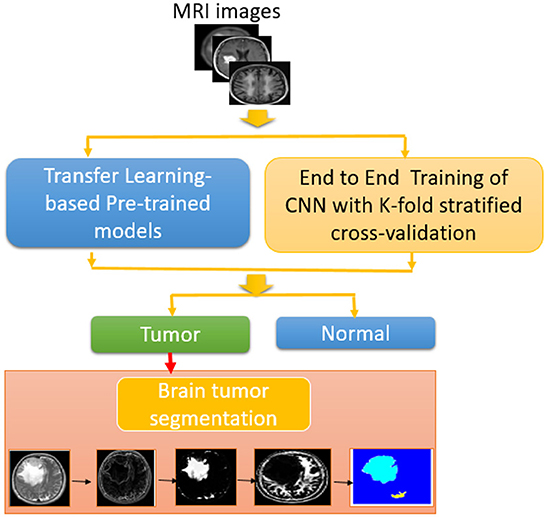
Artificial Intelligence (AI) is transforming the landscape of medical diagnostics by providing sophisticated tools for cancer prediction. In the context of pediatric gliomas, AI algorithms can analyze complex patterns in medical imaging, such as MRIs, to help identify subtle changes that may signal a recurrence. The study highlighted in the introduction demonstrates that an AI model using temporal learning significantly outperforms traditional methods, showcasing the potential of AI to enhance prediction accuracy for brain cancer recurrence.
By integrating large datasets from multiple scans over time, AI can learn and detect nuances in tumor behavior that might be missed by human observers. This capability is especially beneficial in pediatric patients, where traditional follow-up routines can be intensive and stressful. With AI’s growing role in cancer prediction, there’s hope that personalized treatment plans can be devised more swiftly and accurately, ultimately leading to better outcomes for children undergoing treatment for brain tumors.
Temporal Learning in AI Models for Cancer Recurrence Prediction
Temporal learning is a groundbreaking technique that leverages time-sensitive data to enhance the predictive capabilities of AI models. In the study, researchers applied temporal learning to develop an AI model that analyzes a series of MRIs taken post-treatment to track changes in gliomas. This approach allows the model to create an evolving picture of the tumor’s behavior, offering insights into how it may respond to treatment or whether it’s at risk of recurrence.
One of the findings of the study was that when the model was provided with a sequence of images, it could predict cancer recurrence with an impressive accuracy of 75-89%. This is a significant improvement compared to traditional methods, which relied on single scans and achieved an accuracy comparable to random guessing. The implications of this enhanced predictive power are profound, as it could lead to more tailored treatment regimens that respond to patients’ unique tumor profiles, reducing unnecessary stress on families while ensuring those at higher risk receive appropriate care.
Advancements in Brain Cancer Imaging Techniques
Recent advancements in brain cancer imaging techniques have played a pivotal role in enhancing our ability to monitor pediatric gliomas. Improved imaging modalities, such as high-resolution MRIs and advanced functional imaging, provide crucial information about tumor characteristics, progression, and response to therapy. These techniques are invaluable in the clinical setting, aiding healthcare professionals in making informed decisions about treatment protocols and follow-up strategies.
With the integration of AI and more sophisticated imaging technology, clinicians can now utilize brain cancer imaging not just for diagnosis or immediate treatment planning, but also for ongoing surveillance of recurrence risk. This reflects a shift towards a more proactive approach in managing pediatric brain tumors, allowing for timely interventions and reducing the frequency of imaging for lower-risk patients. Advances in imaging are not only improving patient care but also enabling researchers to gather extensive data that can further refine predictive models.
Assessing Recurrence Risk in Pediatric Brain Tumors
Assessing the risk of recurrence in pediatric brain tumors is a complex process that demands a multifaceted approach. Traditional methods rely heavily on clinical assessments and imaging results, leading to potential gaps in accurately identifying high-risk patients. As outlined in the aforementioned study, the use of AI and temporal learning represents a revolutionary step forward, allowing healthcare providers to pinpoint recurrence risk more effectively and in a less invasive manner.
With accurate recurrence risk assessment, clinicians can prioritize follow-up care and tailor treatment strategies to each patient’s unique circumstances. Lower-risk patients may benefit from reduced imaging frequency, sparing them and their families from the psychological burdens associated with frequent scans, while high-risk individuals can receive more intensive monitoring and timely interventions. This personalized strategy marks a significant advancement in pediatric oncology, highlighting the necessity for innovations that improve patient outcomes.
Next Steps: Implementing AI in Clinical Trials
The promising results of AI-driven models necessitate further investigation through clinical trials aimed at validating their efficacy in real-world settings. Researchers are eager to explore how these advanced tools can be integrated into existing treatment frameworks to enhance patient care in pediatric glioma cases. Clinical trials will allow for meticulous evaluation of the benefits of AI in reducing imaging frequency for lower-risk patients, while simultaneously ensuring adequate monitoring for those identified as high-risk.
These trials will not only assess the predictive accuracy of the AI models but also examine the impact of AI-informed decisions on treatment outcomes. By carefully managing and analyzing patient data, researchers hope to establish standardized protocols that leverage AI for enhanced risk stratification, ultimately leading to improved survival rates and better quality of life for pediatric patients battling brain cancer.
Impact of Healthcare Innovations on Pediatric Oncology
Healthcare innovations, especially in the realm of cancer treatment, are continually reshaping the landscape of pediatric oncology. With the adoption of AI, telemedicine, and advanced imaging techniques, practitioners are now armed with more powerful tools for diagnosing and managing childhood cancers. These innovations not only have the potential to improve clinical outcomes but also to alleviate the emotional and logistical burdens faced by families during treatment journeys.
Moreover, collaboration between researchers, healthcare institutions, and technology developers is critical to advancing these innovations. As studies like the one conducted at Mass General Brigham gain traction, funding opportunities and institutional support will likely foster more groundbreaking research. The integration of AI and modern imaging into pediatric oncology care signifies a step toward more compassionate and effective healthcare solutions that prioritize patient wellbeing alongside clinical efficacy.
Challenges and Future Directions in AI Research for Cancer Prediction
Despite the exciting potential of AI in predicting cancer recurrence, several challenges remain. Researchers must address issues related to data quality, algorithm bias, and the need for extensive validation in diverse clinical settings. The transition from experimental findings to practical applications involves ensuring that AI models can be reliably used across various healthcare facilities without compromising their predictive accuracy.
Future research will need to focus not only on refining AI algorithms and enhancing data collection but also on developing frameworks for clinician training and patient education surrounding AI technologies. This holistic approach will help integrate AI solutions into healthcare sustainably, ensuring both medical personnel and patients feel confident and supported when engaging with AI-driven tools for cancer prediction.
The Role of Support Systems for Families Navigating Brain Cancer
Navigating a pediatric brain cancer diagnosis is undoubtedly challenging for patients and their families, often leading to emotional and financial strain. Support systems play a crucial role in helping families cope with the challenges posed by treatment and follow-up procedures. Medical social workers, psychological counseling, and community support programs provide vital resources and networks that assist families in managing their concerns as they go through this tumultuous experience.
Furthermore, with advancements in technologies such as AI aiding in the prediction of recurrence risk, families can find some solace in having clearer insights into their child’s condition. Knowing whether their child may require more intensive monitoring or can afford to take a less aggressive approach to follow-up care can significantly alleviate stress for families, allowing them to focus their energies on support and recovery. Building resilient, supportive environments is essential to improving outcomes and quality of life for children battling brain cancer.
Frequently Asked Questions
How does AI contribute to predicting brain cancer recurrence in pediatric patients?
AI plays a vital role in predicting brain cancer recurrence in pediatric patients by utilizing advanced algorithms that analyze multiple brain scans over time. This approach enhances accuracy compared to traditional methods, allowing for better risk assessment and early detection of potential relapses.
What is temporal learning in the context of predicting brain cancer recurrence?
Temporal learning is a technique that trains AI models to analyze sequences of brain scans taken over time. By identifying subtle changes across these scans, the model improves its ability to predict brain cancer recurrence, particularly for pediatric gliomas, enhancing overall patient care.
Why are traditional methods less effective in predicting recurrence risk for pediatric gliomas?
Traditional methods rely on single imaging studies, which only provide a snapshot of the patient’s condition. This limited perspective can lead to inaccurate predictions regarding brain cancer recurrence. In contrast, AI tools utilizing temporal learning analyze multiple scans to draw more reliable conclusions.
Can AI improve the frequency of imaging needed to monitor brain cancer recurrence?
Yes, AI has the potential to tailor the frequency of imaging needed for monitoring brain cancer recurrence. By accurately predicting which patients are at lower risk, those patients may require less frequent scans, reducing the burden on families and enhancing the overall care process.
What are the implications of using AI in brain cancer imaging for pediatric glioma treatment?
The use of AI in brain cancer imaging for pediatric glioma treatment could lead to improved risk assessment for recurrence, allowing healthcare providers to strategize treatment plans more effectively. This could mean preemptive treatment for high-risk patients or reduced surveillance for those at lower risk.
What level of accuracy did the AI model achieve in predicting brain cancer recurrence?
The AI model utilizing temporal learning achieved an impressive accuracy of 75-89% in predicting brain cancer recurrence within one year post-treatment for both low- and high-grade gliomas, significantly outperforming traditional single image predictions.
What is the significance of the National Institutes of Health in this AI research?
The National Institutes of Health partially funded this research, highlighting its importance in advancing AI technology for medical applications. Their support underscores the potential for AI tools to revolutionize the approach to predicting brain cancer recurrence and improving patient outcomes.
How might AI-defined risk predictions change clinical practice for pediatric glioma patients?
AI-defined risk predictions might change clinical practice by optimizing follow-up care for pediatric glioma patients. This could reduce unnecessary imaging for those at lower risk while ensuring that high-risk patients receive timely and targeted therapies to manage recurrence more effectively.
Are there any limitations to the current AI methods for predicting brain cancer recurrence?
While promising, current AI methods for predicting brain cancer recurrence still require further validation in diverse clinical settings. Researchers caution that broader applications depend on extensive testing to ensure reliability and effectiveness across various patient populations.
What future developments are expected in AI and brain cancer imaging for recurrence prediction?
Future developments in AI and brain cancer imaging for recurrence prediction may include clinical trials that assess the real-world impact of AI-informed decisions on treatment planning and patient outcomes, paving the way for enhanced care strategies and improved survival rates.
| Key Points | Details |
|---|---|
| AI Prediction Tool | An AI tool trained on brain scans outperformed traditional methods in predicting relapse in pediatric brain cancer patients. |
| Study Background | The study was conducted at Mass General Brigham and published in The New England Journal of Medicine AI. |
| Technique Used | Researchers used temporal learning to analyze longitudinal scans, improving prediction accuracy for cancer recurrence. |
| Accuracy of Predictions | The model achieved an accuracy rate of 75-89% compared to traditional methods at around 50%. |
| Goals of Research | To reduce follow-up imaging stress for children and better identify those at high risk for recurrence. |
| Future Applications | Plans for clinical trials to validate AI predictions and their usefulness in treatment planning. |
Summary
Predicting brain cancer recurrence has become a vital focus in improving pediatric care, especially for those diagnosed with gliomas. A groundbreaking study has revealed that an AI tool analyzing multiple brain scans can predict relapse risks with higher accuracy than traditional methods. This technology aims to enhance the quality of care by identifying high-risk patients more effectively and reducing the psychological burden of extensive imaging on families. As further research unfolds, the hope is to integrate these AI-driven insights into clinical practice to optimize treatment strategies.