TIM-3 Therapy for Alzheimer’s is pioneering a new frontier in Alzheimer’s treatment by harnessing the body’s immune system to combat the disease. Recent research shows that targeting checkpoint molecules like TIM-3 can rejuvenate microglia function, enabling these brain immune cells to clear harmful plaques that contribute to memory decline. By inhibiting the TIM-3 molecule, scientists have observed cognitive improvement in mouse models, providing hope for future therapies in humans that may restore memory and cognitive functions. This innovative approach not only focuses on the plaque removal but also emphasizes the intricate relationship between the immune system and Alzheimer’s. As we seek effective therapies for this debilitating condition, TIM-3 Therapy could lead to groundbreaking advancements in our understanding of how to utilize our immune system to fight Alzheimer’s.
The TIM-3 treatment for Alzheimer’s disease represents a strategic shift in addressing cognitive decline associated with age-related conditions. This therapy utilizes an immune checkpoint inhibitor that plays a crucial role in regulating brain immune responses, particularly through enhancing the functionality of microglia cells. Recent studies indicate that diminishing the expression of TIM-3 on these immune cells facilitates the clearance of amyloid plaques, which are detrimental to cognitive health. Consequently, the potential for cognitive recovery opens a new discourse on immune-mediated strategies in the realm of neurodegeneration. By targeting these intricate mechanisms, this innovative therapy not only aims to improve cognitive performance but also seeks to redefine our approach to treating Alzheimer’s.
Understanding the Role of Microglia in Alzheimer’s Disease
Microglia are the primary immune cells of the central nervous system, playing critical roles in maintaining brain health. In the context of Alzheimer’s disease, their function is particularly vital. These cells not only help in the clearance of amyloid plaques, which are characteristic of Alzheimer’s, but they also regulate synaptic pruning during development. When microglia become dysfunctional, they fail to clear these plaques effectively, leading to the cognitive decline associated with Alzheimer’s. Recent research indicates that the expression of checkpoint molecules like TIM-3 inhibits the ability of microglia to perform their clearing functions.
As Alzheimer’s progresses, microglia become increasingly homeostatic, meaning they cease their proactive role in clearing debris. This change is exacerbated by the elevated levels of TIM-3 expression observed in these cells within Alzheimer’s patients. Consequently, instead of engaging actively in plaque removal, microglia become quiescent, contributing to the progression of the disease. Understanding these mechanisms is crucial, as they highlight potential targets for therapeutic interventions aimed at restoring normal microglial function.
TIM-3 Therapy for Alzheimer’s: A Potential Breakthrough
Recent studies have identified TIM-3 as a promising target for Alzheimer’s therapy due to its role in inhibiting microglial activity. By deleting the gene responsible for producing TIM-3 in experimental models, researchers observed a marked improvement in cognitive functions and a reduction in plaque accumulation. This suggests that TIM-3 therapy could potentially reactivate the plaque-clearing abilities of microglia, offering a novel approach to treatment. Such therapy might involve the use of anti-TIM-3 antibodies or small molecules designed to block the inhibitory effects of TIM-3.
The implications of TIM-3 therapy are extensive, especially given the challenges faced by traditional Alzheimer’s treatments. While many therapies have aimed at amyloid beta clearance and have shown limited success, targeting TIM-3 could address the underlying reasons for plaque persistence. Enhancing microglial function could improve cognitive outcomes, making this approach revolutionary in Alzheimer’s treatment. Continued research, including preliminary human trials, is essential to understand the potential of TIM-3 inhibitors in clinical settings.
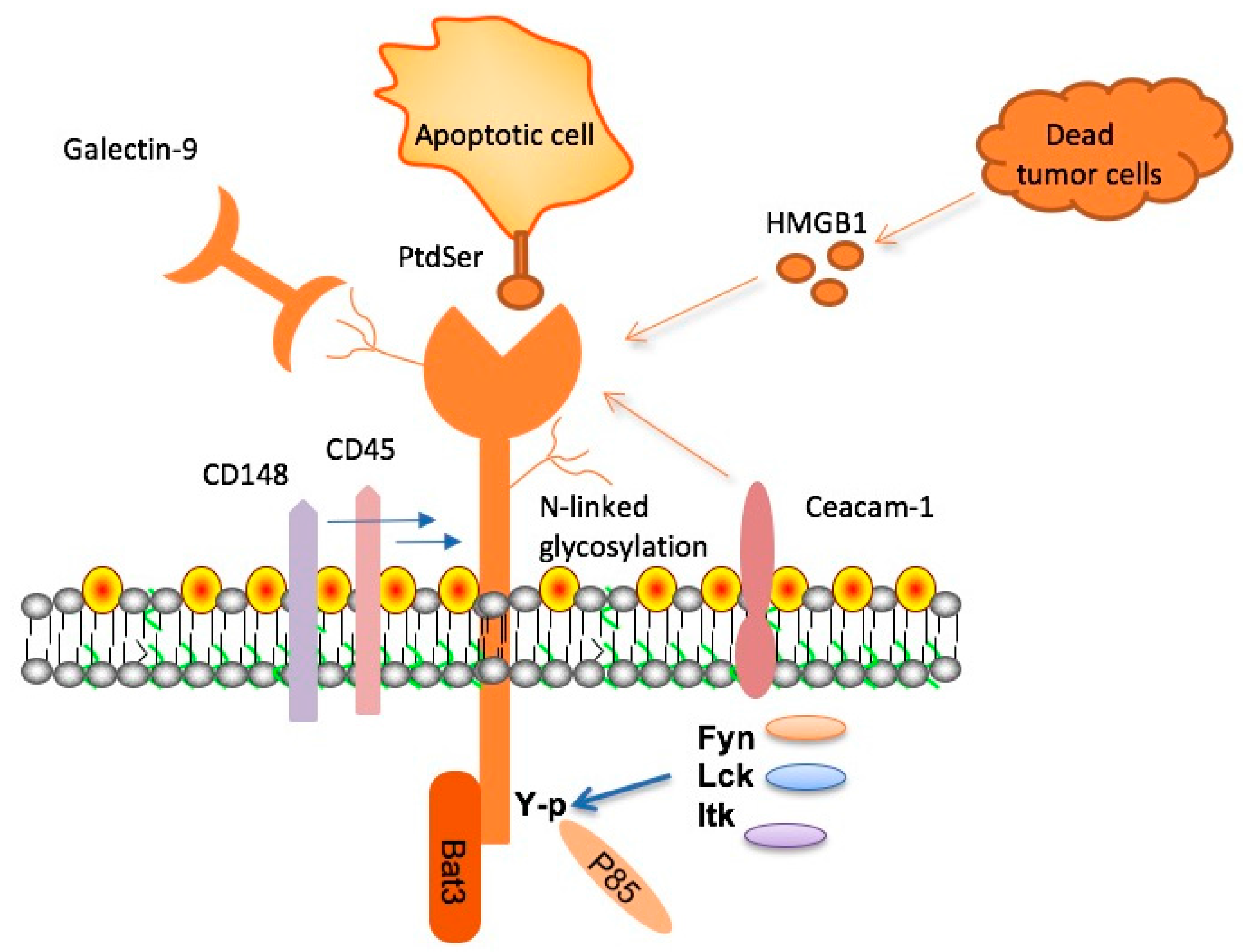
The Mechanism Behind Checkpoint Molecules
Checkpoint molecules, such as TIM-3, are critical regulators of the immune response and have recently come under scrutiny for their role in neurodegenerative diseases like Alzheimer’s. In healthy immune function, these molecules serve to prevent overactivity of immune cells, maintaining homeostasis within the body. However, in the context of Alzheimer’s, TIM-3 has been found to hinder the activity of microglia, preventing them from clearing toxic amyloid plaques. This dual nature of checkpoint molecules shows their importance not only in cancer immunology but also in neurodegenerative conditions.
The regulation of microglial activation through checkpoint molecules provides insights into potential therapeutic avenues. By understanding how TIM-3 and similar molecules function, researchers can develop strategies to manipulate these pathways to rejuvenate microglial activity. In essence, disabling TIM-3’s inhibitory signal could reinvigorate the microglia’s ability to eliminate detrimental plaque build-up, thus altering the course of Alzheimer’s disease pathology.
Impacts of Alzheimer’s on Memory and Behavior
Alzheimer’s disease significantly impacts memory and behavior, primarily due to the buildup of amyloid plaques and neurofibrillary tangles in the brain. As these proteins accumulate, they disrupt synaptic communication and impair the fundamental processes involved in memory formation and retrieval. This disruption leads to the characteristic cognitive decline seen in Alzheimer’s patients, manifesting in forgetfulness, confusion, and behavioral changes such as increased agitation or depression.
Research has demonstrated that interventions targeting plaque clearance can lead to observed improvements in memory-related tasks. For instance, studies using mouse models have shown that cognitive behaviors improve when plaques are reduced or altered through genetic modifications, such as deleting the TIM-3 gene. These findings highlight the potential for therapies aimed at targeting the biological mechanisms behind Alzheimer’s to restore cognitive function and improve quality of life for patients.
Exploring Immune System Contributions to Alzheimer’s
The immune system plays a pivotal role in modulating the effects of Alzheimer’s disease. Microglia, as the brain’s resident immune cells, help maintain a balanced environment and protect against neurodegeneration. However, the dysregulation of microglial function due to checkpoint molecules like TIM-3 can exacerbate Alzheimer’s pathology. Research indicates that boosting immune responses through strategic therapies may enhance the brain’s ability to clear harmful proteins, thereby preserving cognitive health.
Emerging studies are shedding light on how altering immune responses can affect Alzheimer’s progression. By understanding the interplay between immune checkpoints and microglial activity, there’s potential for new treatment paradigms that could activate dormant microglial function. This represents a shift in thinking about Alzheimer’s not just as a neurodegenerative disorder but also in terms of immune modulation, suggesting that addressing both inflammation and plaque accumulation may yield better therapeutic outcomes.
Future Directions in Alzheimer’s Research
The future of Alzheimer’s research is poised for exciting developments, especially with the increasing focus on immune modulation therapies such as TIM-3 inhibitors. The recent successes in murine models show promise for translating these findings into human clinical trials. As researchers continue to elucidate the complex mechanisms behind microglial dysfunction and plaque formation, it becomes evident that innovative strategies can be developed to target the root causes of the disease.
Furthermore, the collaborative efforts between immunologists and neurologists are crucial in this endeavor. By merging insights from the fields of immunology and neurobiology, researchers can develop multifaceted approaches for Alzheimer’s treatment that not only inhibit plaque formation but also enhance cognitive function. This integrative model could pave the way for a new era in Alzheimer’s therapy, focusing on restoring immune balance and cognitive capabilities.
Restoring Cognitive Function in Alzheimer’s Patients
One of the crucial challenges in Alzheimer’s therapy is restoring cognitive function and slowing disease progression. The identification of TIM-3 as a critical inhibitory molecule present in microglia has opened up new avenues to explore how these immune cells can be mobilized to improve cognition. By targeting TIM-3, researchers aim to enhance microglial activity, enabling them to effectively clear plaques and restore neural circuitry associated with memory and learning.
Experimental therapies focusing on cognitive improvement have shown promising results in animal models, with interventions leading to partially restored memory capabilities. If similar outcomes can be replicated in human clinical trials, the potential to significantly improve quality of life for Alzheimer’s patients becomes feasible. Ongoing studies aim to assess the efficacy and safety of such treatments, emphasizing a bright outlook for future cognitive rehabilitation strategies.
Alzheimer’s Treatment Strategies: From Concepts to Clinics
Alzheimer’s treatment strategies are evolving as new research reveals promising targets for intervention. Historically, therapies have primarily aimed at managing symptoms rather than addressing the underlying mechanisms of the disease. However, recent studies have shifted focus towards more innovative strategies that aim to restore normal microglial function, such as targeting checkpoint molecules like TIM-3. This transition from conceptual ideas to practical applications in clinical settings represents a significant advancement in Alzheimer’s treatment.
As research progresses, the potential for new pharmacological agents that can specifically boost immune responses in the brain becomes increasingly tangible. Refinements in understanding how to manipulate these pathways will be crucial in developing effective treatments. By focusing on therapies that promote cognitive function and overall brain health, it is possible to provide Alzheimer’s patients with more than just symptomatic relief; these strategies could address the fundamental pathology of the disease.
Challenges in Alzheimer’s Drug Development
Developing effective drugs for Alzheimer’s disease is fraught with challenges. Traditional drug trials have often resulted in disappointing outcomes, with many therapies failing to show significant cognitive improvements in patients. Part of the underlying issue is the complexity of Alzheimer’s pathology, which includes multifactorial components like amyloid accumulation, tau tangles, and inflammatory responses. Addressing these overlapping features requires a nuanced understanding of the disease.
Moreover, the transition from promising laboratory results to clinical efficacy remains a daunting hurdle. With the exploration of TIM-3 therapy, there’s hope for a more targeted approach that could enhance the function of microglia and offer tangible benefits for cognitive health. However, ongoing research will be critical in overcoming the historical pitfalls of Alzheimer’s drug development and paving the way for successful therapeutics that address the multifaceted nature of the disease.
The Importance of Collaborative Research in Alzheimer’s
Collaboration across scientific disciplines is essential for advancing Alzheimer’s research. By integrating expertise from immunology, neurology, and pharmacology, researchers can create a more comprehensive approach to understanding and treating this complex disease. For instance, the development of TIM-3 inhibitors showcases how combining insights from both immune system behavior and neurological functions can lead to innovative therapeutic strategies.
Interdisciplinary collaboration also fosters the sharing of ideas, resources, and methodologies, enhancing the pace and quality of research. As researchers pool their knowledge and skills, their collective efforts can lead to breakthroughs that individual studies may not achieve. This collaborative spirit is paramount for tackling the urgent challenge posed by Alzheimer’s and transforming potential discoveries into practical, effective treatments.
Frequently Asked Questions
What is TIM-3 Therapy for Alzheimer’s and how does it work?
TIM-3 Therapy for Alzheimer’s focuses on inhibiting the TIM-3 checkpoint molecule, which prevents microglia—the brain’s immune cells—from effectively clearing amyloid plaques. By blocking TIM-3, this therapy aims to enhance microglial function and promote cognitive improvement in Alzheimer’s patients.
How does TIM-3 relate to the immune system in Alzheimer’s disease?
TIM-3 is a checkpoint molecule that regulates the immune response. In Alzheimer’s, TIM-3 expression on microglia is increased, which inhibits their ability to remove harmful plaques. Therefore, TIM-3 Therapy aims to modify this behavior, allowing microglia to better combat the buildup of amyloid plaques.
What are the potential benefits of TIM-3 Therapy for Alzheimer’s treatment?
The potential benefits of TIM-3 Therapy for Alzheimer’s include improved clearance of amyloid plaques by microglia, which could lead to cognitive enhancement and a reduction in Alzheimer’s-related symptoms, increasing overall quality of life for patients.
Can TIM-3 Therapy lead to cognitive improvement in Alzheimer’s patients?
Yes, studies have shown that deleting the TIM-3 gene in mouse models leads to enhanced microglial activity, which not only clears amyloid plaques more effectively but also results in measurable cognitive improvement in memory tasks.
What role do microglia play in TIM-3 Therapy for Alzheimer’s?
Microglia function as the brain’s immune cells and play a critical role in TIM-3 Therapy. By inhibiting TIM-3, these cells are activated to attack and clear amyloid plaques, which is essential for restoring cognitive function in Alzheimer’s disease.
Is TIM-3 Therapy a viable option for all Alzheimer’s patients?
Currently, TIM-3 Therapy is being researched and is not yet available as a general treatment. It shows promise particularly for late-onset Alzheimer’s cases, as TIM-3 has been identified as a genetic risk factor for this type of the disease.
What are checkpoint molecules and how do they affect Alzheimer’s treatment?
Checkpoint molecules, like TIM-3, regulate the immune response by inhibiting immune cell activation. In Alzheimer’s treatment, targeting these molecules can enhance the immune system’s ability to combat amyloid plaques, potentially leading to better therapeutic outcomes.
How does TIM-3 Therapy differ from traditional Alzheimer’s treatments?
Unlike traditional Alzheimer’s treatments that primarily focus on managing symptoms, TIM-3 Therapy aims to address the underlying immune mechanisms by promoting the activation and efficiency of microglia to clear plaques and restore cognitive functions.
What research supports the effectiveness of TIM-3 Therapy for Alzheimer’s?
Research published in Nature highlights that deleting the TIM-3 gene in Alzheimer’s mouse models led to improved memory and plaque clearance, providing a strong foundation for exploring TIM-3 Therapy in human patients.
When can we expect TIM-3 Therapy for Alzheimer’s to be available to patients?
While TIM-3 Therapy shows great promise, further clinical trials and research are necessary to establish its safety and efficacy in humans. It is currently being tested in mouse models with the aim of eventually transitioning to human clinical studies.
| Key Points |
|---|
| TIM-3 is an immune system checkpoint molecule linked to late-onset Alzheimer’s disease, affecting 90-95% of cases. |
| Microglia, the brain’s immune cells, are inhibited by TIM-3, preventing them from clearing amyloid plaques associated with Alzheimer’s. |
| Research demonstrates that deleting the TIM-3 expression in lab mice leads to improved cognitive function and plaque clearance. |
| Potential TIM-3 therapies could involve anti-TIM-3 antibodies to enhance microglia’s ability to attack Alzheimer’s plaques. |
| Ongoing research aims to develop therapies that can effectively halt plaque development in Alzheimer’s disease models. |
Summary
TIM-3 Therapy for Alzheimer’s is a promising avenue in addressing this neurodegenerative disease. By understanding the inhibitory role of the TIM-3 molecule on microglia, researchers are exploring therapies that could reactivate these essential immune cells, thereby enabling them to clear the amyloid plaques that characterize Alzheimer’s. This innovative approach has already shown potential through experiments with genetically modified mice, leading to improved cognitive outcomes. If successful, TIM-3 therapy could represent a significant breakthrough in the treatment of Alzheimer’s disease, providing hope for millions affected by this condition.