Medical research funding is crucial for advancing healthcare and ensuring patient safety in research. Without adequate resources, studies that involve human participants can be jeopardized, leaving gaps in critical oversight like IRB governance. Significant funding cuts, such as the recent freeze of over $2 billion in federal grants, pose a grave risk to the ability of researchers to conduct ethical and thorough clinical trials. These financial limitations not only threaten research integrity but can also hinder the overall progress of innovative treatments that rely on well-funded NIH research grants. As we continue to explore the impact of funding cuts, it becomes clear that maintaining robust investment in medical research is vital for fostering trust and safety in research involving human subjects.
Securing financing for health-related research is essential for fostering advancements in patient care and ensuring ethical practices in clinical studies. Inadequate funding can lead to interruptions in vital oversight mechanisms such as Institutional Review Board (IRB) assessments, ultimately compromising patient safety. The ramifications of financial shortfalls, particularly in the context of federal grant allocations, highlight the interconnectedness of clinical trials and sponsorship. Moreover, these obstacles to funding can exacerbate public skepticism about research practices, emphasizing the importance of safeguarding patient welfare through sustained financial support. As we delve deeper into the conversation about funding in medical research, it is imperative to recognize the profound implications that cuts or restrictions in these areas can have on the health of communities.
The Critical Role of Medical Research Funding
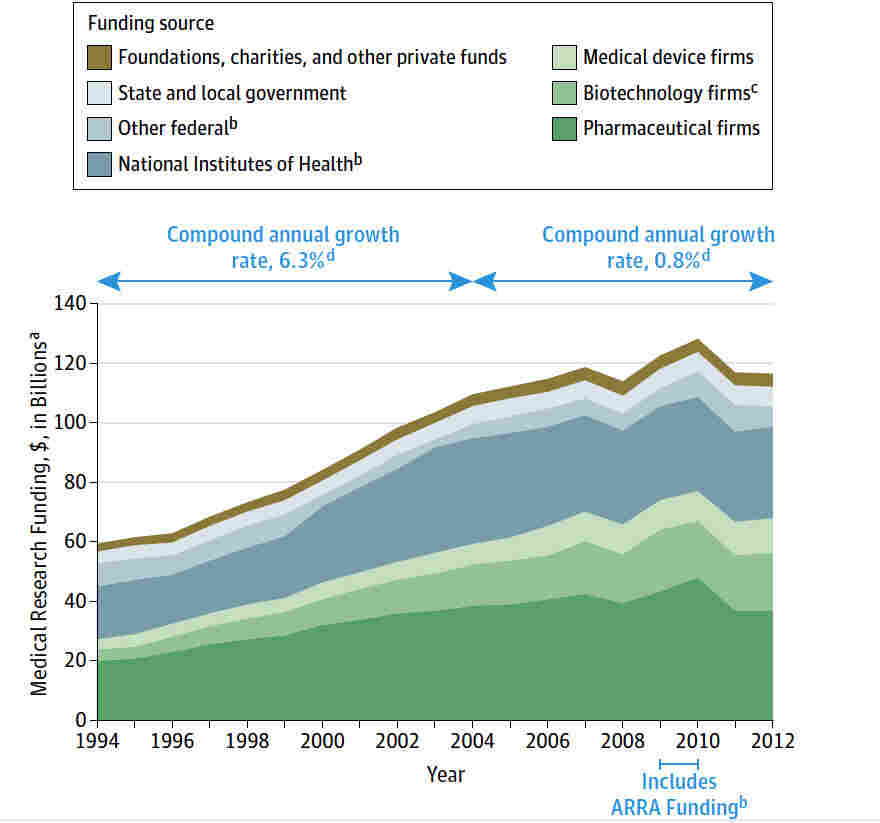
Medical research funding is the lifeblood that sustains numerous health initiatives, fostering innovation and discovery that directly impacts patient care and safety. Funding allocations, particularly from institutions like the NIH, are essential for conducting clinical trials, which help translate laboratory findings into effective treatments. Without adequate funding, researchers face barriers that impede their ability to investigate and verify new therapeutic interventions, ultimately affecting patient safety in a profound way. The freeze or reduction of federal research dollars not only stalls current projects but also dampens future exploration, as financial constraints limit recruitment of skilled personnel and the acquisition of necessary resources.
Moreover, the impact of funding cuts on medical research is not merely financial; it reverberates throughout the entire healthcare landscape. As studies are halted or delayed, patient safety becomes compromised due to the lack of oversight and rigorous evaluation that robust funding ensures. Each research dollar spent translates into a commitment to ethical oversight through Institutional Review Boards (IRBs) and adherence to safety protocols. Consequently, a lack of funding could lead to decreased trust in clinical research, as communities become wary of participating in studies that may no longer be held to the highest ethical standards.
Understanding Patient Safety in Medical Research
Patient safety is a paramount concern in medical research, especially given the potential risks associated with clinical trials. The role of IRBs is critical as they scrutinize research proposals to safeguard participant welfare. They assess various elements, including the informed consent process, risk mitigation strategies, and overall study design, to ensure that the rights and safety of participants are prioritized. This oversight is essential for maintaining public confidence in the research system and ensuring that individuals are not exposed to unnecessary harm whilst contributing to scientific advancement.
However, when funding for IRBs and related oversight mechanisms is cut, the consequences can be severe. Diminished resources can lead to less rigorous oversight and inadequate review processes, thereby endangering patient safety. Communities which rely on the outcomes of clinical trials may suffer from late or ineffective treatments, amplifying existing health disparities. Therefore, robust medical research funding not only undergirds the integrity of research practices but also plays a significant role in protecting human subjects enrolled in studies.
The Damaging Effects of Funding Cuts on Research Efforts and Patient Oversight
Funding cuts have far-reaching implications for research initiatives aimed at ensuring patient safety. When federal research funding is suspended or reduced, the resources available for independent oversight bodies like IRBs become strained. This can lead to less scrutiny of ongoing clinical trials and a hesitance from institutions to undertake new research projects, as the burden of regulatory compliance becomes daunting with limited financial support. Consequently, the quality and effectiveness of patient protection measures may suffer, leaving individuals vulnerable during the research process.
In instances where research studies encounter financial obstacles, the impact extends beyond immediate delays. Participants who engage in clinical trials expecting to receive cutting-edge treatments may experience uncertainty and distress, undermining their trust in the medical research enterprise. As outlined previously, the relationship between funding and patient safety cannot be overstated. Without adequate financial support, clinical trials may falter, compromising not just individual safety but the overall advancement of medical knowledge.
The Importance of IRB Oversight in Clinical Research
Institutional Review Boards (IRBs) provide an essential layer of oversight in clinical research by ensuring compliance with ethical standards and federal regulations. They serve a crucial function in protecting the rights and welfare of research participants by reviewing study protocols and monitoring ongoing research. This oversight helps to mitigate risks to participants and fosters a culture of safety and ethical conduct in clinical trials.
However, if funding for IRBs is cut, their capacity to fulfill these responsibilities may be adversely affected. This can lead to hasty reviews, insufficient monitoring of research compliance, and increased potential for participant harm. With the stakes so high, it is vital that sufficient resources are allocated to support IRBs in their mission of safeguarding participants and ensuring that medical research meets the highest ethical standards.
Impact of NIH Research Grants on Patient Safety
NIH research grants play a pivotal role in advancing studies that uphold patient safety by enabling comprehensive oversight and ethical research practices. These grants not only fund the actual research but also support the infrastructure necessary for rigorous IRB evaluations and adherence to safety protocols throughout the research lifecycle. Therefore, sufficient funding through NIH is not simply a budgetary necessity but a fundamental requirement for protecting participants involved in medical research.
When funding decreases, the ripple effect can jeopardize patient safety, as institutions may be forced to scale back or put a halt to critical research initiatives. The direct correlation between stable funding and the effectiveness of IRB oversight must be acknowledged, as it directly affects the quality of patient engagement and the integrity of consent processes. Advocacy for sustained NIH funding is thus crucial for maintaining high standards of safety in clinical research.
Long-term Consequences of Research Funding Cuts on Patient Trust
The long-term consequences of sustained funding cuts in medical research are profound, particularly regarding public trust in clinical trials and medical innovations. As research efforts become stymied due to financial limitations, potential study participants may become wary of engaging with research initiatives, believing that they may no longer uphold rigorous ethical standards. This erosion of trust can ultimately lead to lower enrollment rates in clinical studies, impeding the progression of critical research that relies on diverse participant populations to validate findings.
Healing the rift created by funding cuts necessitates not just restored financial resources but also a concerted effort to communicate effectively with communities about the measures being taken to ensure patient safety. Transparency in the research process and steadfast commitment to ethical oversight through IRBs can help rebuild confidence among potential participants and encourage greater engagement in future studies.
Reshaping the Landscape of Medical Research Oversight
In an era marked by rapid technological advancements and increasing complexity in disease treatment, the landscape of medical research oversight must also evolve. Robust funding is essential to ensure that oversight bodies like IRBs have the resources to adapt to changing regulatory environments and emerging ethical challenges. This adaptation is key to reinforcing patient safety amidst a landscape where research evolves quickly and the need for safe, compliant protocols grows.
Future efforts must prioritize the allocation of funding to sustain and enhance the oversight infrastructure. Investing in continuous training for IRB members and adopting new technologies to streamline reviews can help foster a more effective and responsive oversight system. As the medical research landscape shifts, embracing these changes will be crucial in protecting patient welfare and maintaining public trust in research.
The Interplay Between Funding, Research Ethics, and Patient Safety
The complex interplay between research funding, ethical standards, and patient safety must be emphasized in discussions about medical research. Ethical oversight does not occur in a vacuum; it hinges on the availability of resources to support the operational needs of IRBs and related agencies. When adequate funding is available, the ability to conduct thorough reviews and ensure participant protection flourishes; conversely, funding cuts can lead to serious ethical lapses that may compromise patient safety.
This relationship highlights the urgent need for stakeholders in the medical research community to advocate for financing that underpins ethical research practices. By championing the importance of sustained research funding, researchers, policymakers, and community members can work together to safeguard not only the integrity of medical studies but also the health and safety of the users who stand to benefit from the advancements made through research.
Building Community Engagement in Medical Research
Community engagement is a vital component of conducting ethical medical research and ensuring participant safety. Involving communities in the research process helps to foster transparency and builds trust, which can be eroded by funding cuts that jeopardize oversight practices. Engaging community members allows researchers to better understand the concerns and expectations of potential participants, setting the stage for informed decision-making regarding study participation.
Effective communication and active involvement of community members can mitigate the negative impact that funding disruptions have on public engagement in clinical research. Establishing outreach initiatives that educate communities about the importance of patient safety in research helps empower individuals to take an active role in the research landscape. By prioritizing community engagement, researchers can rebuild trust and encourage participation, despite the challenges posed by funding limitations.
Frequently Asked Questions
How does medical research funding ensure patient safety in clinical trials?
Medical research funding plays a crucial role in ensuring patient safety during clinical trials by supporting rigorous oversight from Institutional Review Boards (IRBs). These bodies review and monitor research protocols to protect participants’ rights and welfare. Adequate funding allows for comprehensive safety assessments, informed consent processes, and ongoing monitoring of adverse events, thus safeguarding participants involved in medical research.
What impact do funding cuts have on patient safety in medical research?
Funding cuts can severely hinder efforts to maintain patient safety in medical research. When research grants are reduced or halted, IRBs may lack the resources needed for thorough oversight, potentially compromising participant welfare. Disruption in funding can lead to delayed studies, increased risks for patients, and heightened public skepticism about research integrity and safety.
How do NIH research grants support patient safety in medical studies?
NIH research grants directly contribute to patient safety by providing the necessary funding for the establishment and functioning of IRBs, which oversee research involving human participants. NIH-funded research must adhere to strict ethical guidelines, ensuring that studies prioritize patient safety through careful monitoring and risk assessment.
What is the role of IRBs in medical research funding and patient safety?
IRBs play a vital role in medical research funding by ensuring that any research project involving human subjects is ethically reviewed and monitored for safety. They assess study designs, risk mitigation strategies, and informed consent processes, ensuring that patient safety remains a top priority throughout the research lifecycle.
How is patient safety maintained in the context of clinical trials and funding?
Patient safety in clinical trials is maintained through a combination of adequate medical research funding and rigorous oversight by IRBs. Funding provides the necessary resources for monitoring studies across multiple sites, ensuring compliance with ethical standards which protect participants. Adequate financial support is essential for fostering an environment where patient safety can be upheld during clinical trials.
What are the consequences of a stop-work order on medical research funding and patient safety?
A stop-work order on medical research funding can have dire consequences for patient safety. It interrupts essential oversight functions of IRBs, limits the ability to add new study sites, and delays the initiation of critical research, all of which can negatively impact participant welfare and undermine public trust in the research process.
Why is it important to maintain funding for IRB oversight in medical research?
Maintaining funding for IRB oversight is critical for ensuring the ethical conduct of medical research. IRBs are responsible for protecting the rights and safety of research participants. Without adequate funding, IRBs may struggle to fulfill their duties, leading to potential risks for participants and raising concerns about the integrity of medical research.
| Key Point | Details |
|---|---|
| Funding Freeze | The Trump administration froze over $2 billion in federal research grants to Harvard, disrupting patient safety efforts in medical research. |
| Impact on IRBs | Institutional Review Boards (IRBs) are essential for reviewing, approving, and overseeing medical research, ensuring compliance and participant safety. |
| Patient Protection | IRBs play a crucial role in safeguarding patients by assessing risks, monitoring data, ensuring informed consent, and maintaining ethical standards. |
| Historical Context | Historical abuses in medical research underscore the need for strict oversight through IRBs to protect study participants’ rights. |
| Consequences of Funding Cuts | Cuts to funding can halt critical studies, erode public trust, and hinder the development of new therapies, risking participant safety. |
Summary
Medical research funding is vital for ensuring patient safety and ethical oversight in clinical studies. The recent federal funding freezes have significant implications for the integrity of research, highlighting the crucial role of Institutional Review Boards (IRBs) in safeguarding participants’ rights. Without adequate funding, ongoing studies face unnecessary halts, compromising not only research outcomes but also public trust in medical research practices. The potential delay in developing new therapies poses a serious risk to patient safety, underscoring the need for stable and reliable medical research funding.